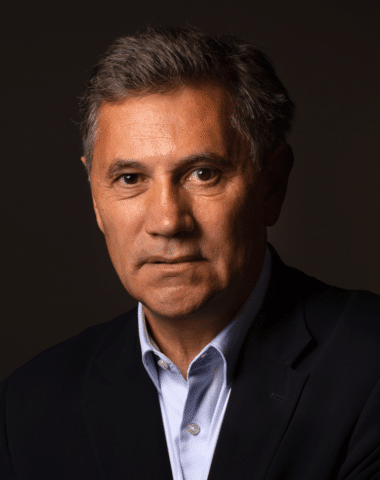
Just as the practice of medicine is more than prescribing medication, personalised medicine more than targeted treatments. Étienne Minvielle, professor at École Polytechnique is working on more personalised healthcare pathways. His aim is to consider patients as a whole, taking into account their social context, habits and even beliefs.
“We’re talking about a personalised approach throughout the the entire journey of a patient through the healthcare system. From hospital to home, including practitioners such as independent nurses and pharmacists,” Minvielle explains.
Offer patients the best guidance
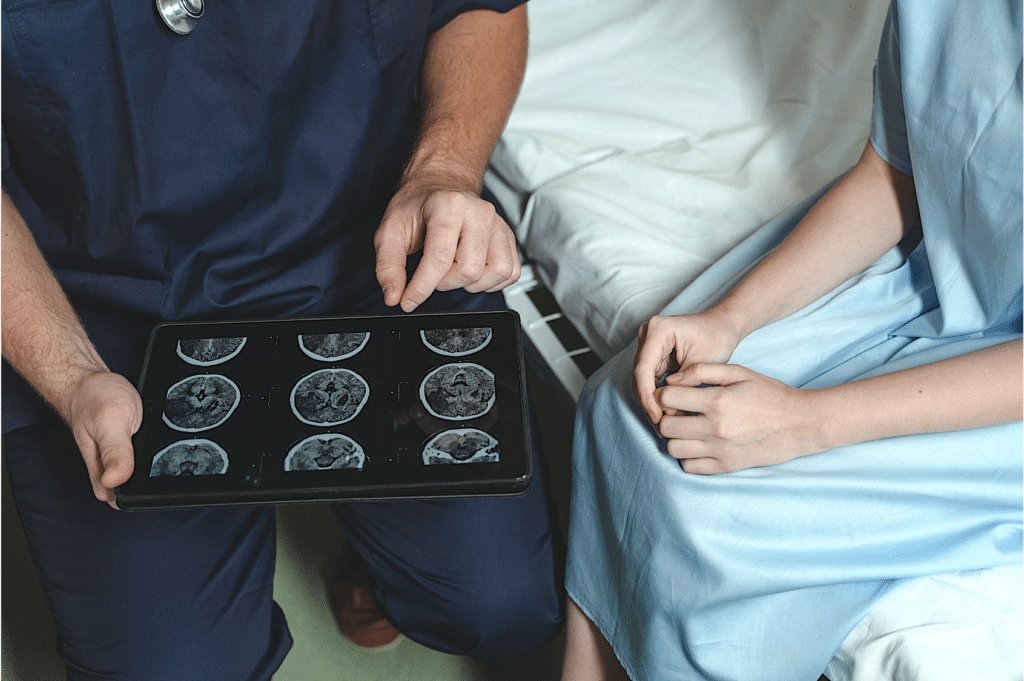
The idea is to draw on tools developed in the service and e‑commerce sectors to tailor customer experience. However, instead of offering discounts based on shopping habits, personalised care means taking into account the patient’s social determinants and psychosocial needs.
“Once diagnosed with a chronic illness, a patient will require services and non-medical interventions to improve their quality of life. This could involve getting a pet-sitter during treatment sessions, help with paperwork to report their long-term condition, or organising transport,” he adds.
A patient’s behaviour and personality also affect the way they relate to healthcare. They might, for example, have a habit of researching health-related information online, tend to engage in risky behaviour, have a positive or negative outlook, be introverted, extroverted, etc. “All of these factors influence the patient’s response,” Minvielle says. In order to take them into account, he is developing patient-centred management models.
These tools require data, and AI can facilitate data collection and help build relevant profiles. “But in health, much of the data is highly complex,” he says. “We’ll need new professionals, such as coordinating nurses, to make sense if it.” Connected objects, such as pill dispensers, could also be used; blood tests could be prescribed to check for metabolites so as to monitor patient compliance. “These solutions must go hand in hand with ethical considerations. How far can we go without intruding on patients’ lives?”
Preserving patient autonomy
When it comes to ethics, vigilance is required on several fronts. “Personalised medicine must not restrict access to care,” Minvielle stresses. “There are risks pertaining to access to personalisation, as well as minority representation in our models.” In a system that adapts patient care pathways to their specific profile, digital models could be used to organise care options into broad categories. This would streamline care pathways, restricting them in a way that may omit less popular preferences within the patient population.
Lastly, personalisation must not come at the expense of patient autonomy. Minvielle believes that “patients should be able to opt out of care pathway personalisation, and choose their own personalisation pathway, even if it is not optimal.”
Human and artificial intelligence
Given what’s at stake, such a program cannot solely rely on digital tools. Human intelligence is required. Minvielle reminds us that “AI cannot yet detect its own errors, whereas a human will immediately notice if a patient has been given the wrong advice.”
Will this system save money? “It remains to be seen. On the one hand, it should reduce waste; on the other, we would be creating a more complex system of care.” Minvielle agrees that more research is needed, and truly personalised care pathways are still some time off.
“The main difficulty is bringing everything together”, he says. The individualisation model is based on research from a number of fields: public health (integrating socioeconomic determinants); psychology (analysing patient behaviour and demands); and medical research (examining the efficacy of treatments on various patient profiles). Yet “all of these groups are working in isolation. If we are to develop a culture of personalisation within the health system, we have to demonstrate its feasibility.”